Cancer Wins Round One
 Thursday, June 9, 2016 at 8:41AM
Thursday, June 9, 2016 at 8:41AM 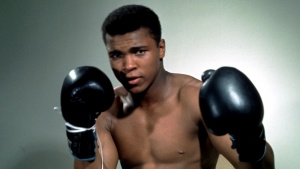 Despite a challenging week of news that not only have the original two tumors grown, but three more have appeared, I find myself at the crossroads of chemo vs clinical trial once again. Cancer may have won round one, but I am not down and out just yet.
Despite a challenging week of news that not only have the original two tumors grown, but three more have appeared, I find myself at the crossroads of chemo vs clinical trial once again. Cancer may have won round one, but I am not down and out just yet.
The next squirmish begins on June 21st with the addition of the drug Pembrolizumab or for us non-medical geeks, Keytruda. The drug is dispensed through infusion, similar to chemo. It is a monoclonal antibody and used in conjunction with my current medication of Acalabrutinib, its function is to stop or slow down the progression of the cancer.
Dr Anderson reassured me that I have not lost ground, but it does feel that way. I was not surprised by having to switch to the study on both drugs, but was discouraged at the news of more tumors. They are extremely small but nonetheless they are there. His words were that without the drug, this would be a crisis and the tumors would have grown exponentially. The fact that the drug was able to keep us at the slower pace of growth is good news, but not enough to bring out the band.
Still, it was discouraging to me and to my family that the past three months have only made small steps forward and what seemingly feels like a few steps back. I can at anytime choose to take chemotherapy. Dr Anderson readily admitted that the tumors are so small that chemo would knock them out quickly. The immunotherapy drugs are slow acting, hence the new growths. It takes the Acalabrutinib three months to show results. But not one to back down from a good fight, I have opted to add the Keytruda and see this to the hopefully meaningful results we need.
Other new horizons in cancer therapies are DNA repair inhibitors, that help chemo's effectiveness by working on the DNA's ability to repair itself. The Nobel Prize was awarded to Paul Modrich, Tomas Lindahl and Aziz Sanca for the mechanistic studies of DNA repair. Which is alot of jargon to say, if we can use immunotherapies to keep the DNA from repairing itself, cancer could be stopped in its tracks. Effective in colon cancer and lung cancer, we are now seeing studies to find applicable patients who have similar DNA repair defects.
All this encourages me to continue the fight and to see what changes are rapidly being made to give cancer the knock out punch, or to at least change the face of the disease from terminal to chronic and keep cancer down for the count.
Feeling a little like Muhammed Ali...float like a butterfly, sting like bee. Cancer, you have not seen the last of me!